Corneal endothelial failure could only be treated with the penetrating keratoplasty (PKP) method. While PKP successfully resolved the corneal failure, vision results after the surgery were poor - many patients required contact lenses or glasses to achieve acceptable vision afterwards. Recovery between surgeries was also long, ranging from six months to two years.
- Home
- History
- Design
- Description
- Impact
Induced Pluripotent Stem Cell Therapy to Treat Corneal Endothelium Damage
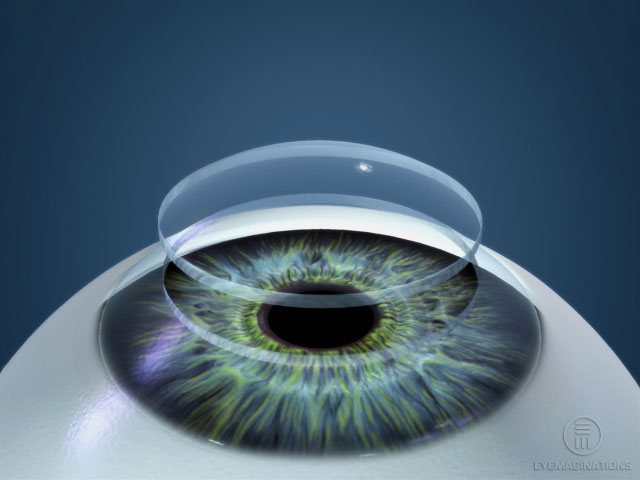
 Over 60 million people suffer every year from blindness and other eye disorders as a result of diseases related to the corneal endothelium, an inner layer of the cornea in the eye. As of now, there is no permanent solution to reverse this damage. However, Induced Pluripotent Stem Cells, or IPSCs, would potentially permanently cure diseases involving the corneal endothelium.
Over 60 million people suffer every year from blindness and other eye disorders as a result of diseases related to the corneal endothelium, an inner layer of the cornea in the eye. As of now, there is no permanent solution to reverse this damage. However, Induced Pluripotent Stem Cells, or IPSCs, would potentially permanently cure diseases involving the corneal endothelium.
History of IPSCs, Stem Cells, and Corneal Endothelial Failure
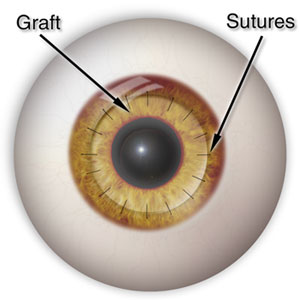
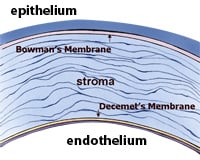
Dr. Gerrit Melles developed a new method for replacing the cornea: deep lamellar endothelial keratoplasty, or DLEK. This method involved a lamellar dissection of Descemet's membrane. However, in 2004, Melles improved his previous technique to involve stripping of Descemet's membrane as opposed to dissection. His new method was called DSEK: Descemet's stripping endothelial keratoplasty.
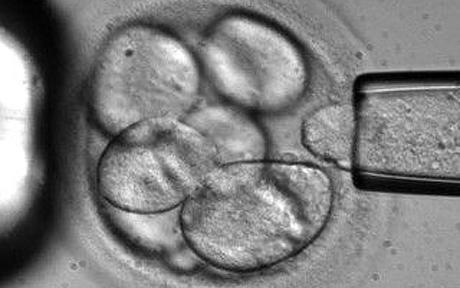
NIH-funded human stem cell research was approved by President Obama. This relatively recent change has allowed scientists to experiment with human stem cells, and progress further in their research towards the regrowth and creation of various parts of a human, in particular the corneal endothelium.
Scientists created an embryonic eye, using stem cells to create a retina-like-structure that can discern varying levels of light. This was an improvement over older experimentation because this retina contained pigment and nerve cells, as well as the addition of molecules found in the environment to simulate an actual eye.
By 2032, scientists will have mastered the use of Induced Pluripotent Stem Cells, being able to easily program them to regenerate into nearly any type of cell. This technique will allow replacing corneal endothelium cells possible, meaning any damaged cells can be regrown.
Designing the Procedure
The corneal endothelium is unable to regenerate itself; current treatment is risky and extremely costly
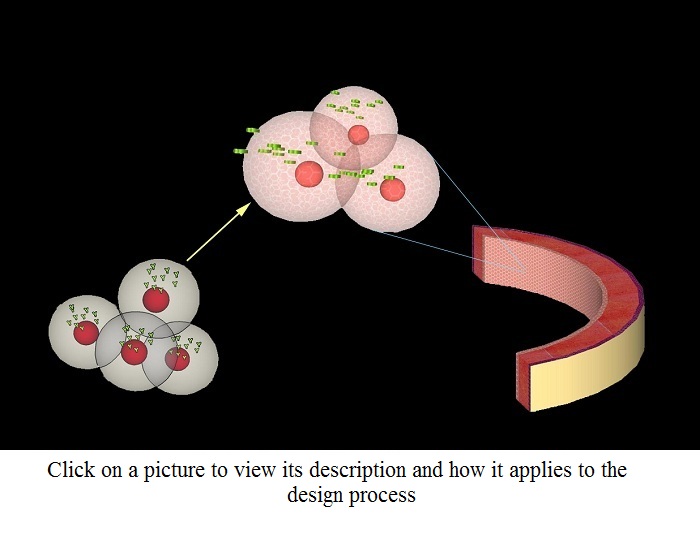
The damaged corneal endothelium is removed
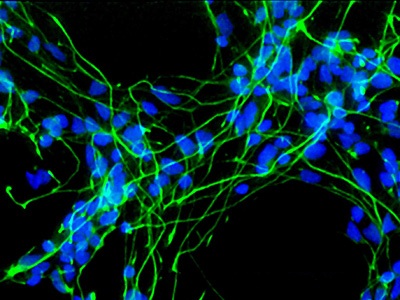
Genetically modified induced pluripotent stem cells (IPSCs) differentiate into corneal endothelium cells, replacing the damaged cells
The cells have been modified so that they will only differentiate in the presence of a unique protein secreted by cells of the corneal endothelium
These differentiated IPSCs replace the corneal endothelium, once again allowing for optical clarity
Fuch's Dystrophy

Fuch's Dystrophy is a degenerative disease occuring when the corneal endthelium fails and its cells die
Consequences include corneal swelling, distorted vision, and eventual blindness
IPSC therapy can replace the damaged corneal endothelial cells, curing the worst effects of Fuch's Dystrophy